Pediatricians frequently recommend melatonin for children with sleep problems, or parents might try it themselves. However, the proper use of melatonin is frequently misunderstood. Here is a guide for parents and pediatricians to decide if a child should try it, and to understand how it should be used. Note: this is a long post so here is a table of contents, so you can find what you need.
- How often are children using melatonin?
- What is melatonin? What does melatonin do?
- How effective is melatonin for sleep problems in children?
- Chronic sleep onset insomnia and Melatonin:
- Autism and Melatonin
- Melatonin and Kids with ADHD
- Delayed Sleep Phase Syndrome and Melatonin
- Children With Neurodevelopmental Delay and Melatonin
- Blindness and Melatonin
- Eczema and Melatonin
- It sounds great. Why should I worry about melatonin?
- My child is already on melatonin. Do I need to freak out?
- My doctor and I have talked about it. What should we consider regarding how and when to give melatonin?
- What is the dose of melatonin for children?
- What is the take home? Should my child take melatonin?
A common thread I find in children coming to Sleep Clinic is that many or all of them have been on melatonin at some point, or are taking it currently. Melatonin is an important tool in the treatment of sleep disorders in children, and because it is naturally derived, there is a widespread perception that it is safe. However, I have become concerned by the frequency of its use, especially in an unsupervised way.
Melatonin sales have doubled in the past ten years, increasing from $90 million in 2007 to $260 million in 2012. Melatonin for children products are being marketed aggressively. I worry that the widespread availability of melatonin has led to some parents using it as a shortcut to good sleep practices. An article in the Wall Street Journal (which also provided the sales figures above), quoted a father’s review on Amazon:
OK, yes, as parents my wife and I should do a better job starting the bedtime routine earlier, turning off the TV earlier, limiting sweets, etc., etc. Well, for whatever reason, this is not our strong suit. This 1 mg light dosage of melatonin is very helpful winding our kids down and getting them ready for bed.
In one regard it is safe— unlike many other medications which cause you to fall asleep, you cannot overdose on it. However, parents need to know that melatonin is a hormone with effects throughout the body and we do not yet know what the long-term effects of melatonin use will be. Many parents in the US would be surprised to know that melatonin is only available with a prescription in the European Union or Australia.
Short on time? Here’s a quick video which should answer most of your questions:
How often are children using melatonin?
It’s hard to know for sure. An article the New York Times, “Parents Are Relying on Melatonin to Help Their Kids Sleep. Should They?”, noted that melatonin sales overall had increased by 87% in the year prior to March 2020. The Times conducted a survey of 933 parents with children under age 18. One third had a history of sleep difficulties in the past year. Over half the parents reported giving melatonin to their children at one time.
What is melatonin? What does melatonin do?
Melatonin is a hormone which is naturally produced by the pineal gland in your brain. It is both a chronobiotic agent, meaning that it regulates your circadian or body clock; and a hypnotic, meaning that at higher doses it may induce sleep. Melatonin is usually used for its hypnotic effect, but it does not have this effect in everyone. Only the chronobiotic effect occurs in all individuals.
The natural rise of melatonin levels in the body 1-3 hours before sleep onset is known as the “dim light melatonin onset” (DLMO). This is the signal involved in body clock scheduling of sleep and corresponds to the end of the “wakefulness” signal produced by the circadian system. Children with insomnia may be given melatonin after their scheduled bedtime passes; what this means is that their bodies are not yet ready for sleep. This is one reason why bedtime fading can be so effective for some children. The doses used clinically (0.5–10 mg or higher) greatly exceed the amount secreted in the body.
There are a few things to be aware of:
- Blue-white light exposure in the evenings shift the DLMO later. This is why bright light exposure in the evenings can worsen insomnia. I highly recommend eliminating ANY screen time for preschool through elementary school children for an hour prior to bedtime. That means no light emitting Kindles, iPads, smartphones, computers, or (God forbid) television in the bedroom For students in junior high and beyond who need to use computers to complete school work, I highly recommend lowering brightness settings and using software to reduce the blue light frequencies. (For more on this read my post about going on a “light diet” here).
- The effect of dosing melatonin (and light therapy for that matter) are phase dependent. What that means is that the timing of giving melatonin determines both the magnitude and direction of effect. Many people do not realize that the optimal time to dose melatonin for shifting sleep period is actually a few hours before bedtime– that is to say, before the DLMO. The other facet of this is that in teenagers with severely shifted sleep schedule (delayed sleep phase syndrome) may actually have a later shift in their sleep schedule if this is not dosed correctly. Thus I would leave the timing of this to a sleep physician. Jet lag is a similar case[1].
- “All natural” melatonin is from cow or pig brains and should be avoided. Most preparations around now are synthetic, which is preferable.
Here’s a short video I put together to explain how when you give the melatonin dose really matters. (Maybe just for the supernerds out there like myself).
How effective is melatonin for sleep problems in children?
The overall effects of melatonin for children include falling asleep more quickly and an increase in sleep time. Like all medicines used to help children fall asleep, there is fairly limited information available. This means that most studies have small groups followed for short periods of time. Furthermore, melatonin not regulated as a pharmaceutical in the U.S. Thus, there is no large pharmaceutical company bankrolling larger and long-term studies (more on this below) . Rather it is regulated as a food supplement by the FDA. For a terrific review, including dosing recommendations, I highly recommend this article by Bruni et al.
Chronic sleep onset insomnia and Melatonin:
Problems with falling asleep are common in children, just like in adults. In children with chronic difficulty falling asleep within 30 minutes of an age-appropriate bedtime. [2] Use of melatonin results in less difficulty with falling asleep, earlier time of sleep onset, and more sleep at night. The initial studies used pretty high doses, but later studies comparing different doses showed that dose didn’t matter, and that the lowest dose studied was as effective as the highest.[3] This is likely due to the fact that ALL these doses were well above the amount produced naturally in the children. Timing between 6–7 PM was more effective than later doses. The authors point out that a midafternoon dose would have the best effect (due to the phase response curve) but that afternoon dosing would have the unpleasant side effective of making children sleepy in the afternoon. (For more info, read here and here and here).
Autism and Melatonin
Sleep problems are common in children with autism. Multiple types of problems occur, including prolonged time to fall asleep, less sleep during the night, and problems with nocturnal and early morning awakenings. Some children with autism have decreased levels of melatonin as well as decreased variation in melatonin secretion throughout the day. Because of this, melatonin has commonly been used in autistic children, which seems to result in less difficulty falling asleep and more sleep at night. Some studies used immediate release preparations, whereas others use long acting forms of melatonin. The majority of studies involved melatonin dosing 30–60 minutes prior to bedtime.
Interestingly, these studies also demonstrated improvement in other domains in some children– specifically, communication, social withdrawal, stereotyped behaviors, and anxiety.
A recent trial looked at a time released melatonin preparation called PedPRM at doses of 2-5 mg. The children in this trial slept 57.5 minutes more (compared with the children who did not receive the medication, who slept 9 minutes more). Most of the benefit seemed to be due to improvement in falling asleep– on average, treated children fell asleep 39 minutes faster. This medication is not yet approved by the FDA but is in the pipeline for approval.
As in other children, melatonin should be added to a behavioral management plan. For pediatricians, there is a great practice pathway which suggests the addition of medication only after a behavioral intervention has failed. Two great resources for families are the Autism Speaks Sleep Toolkit, and the book Solving Sleep Problems in Children with Autism Spectrum Disorders: A Guide for Frazzled Families(affiliate link).
A long acting form of melatonin has shown great promise for children with autism, with children in a 2017 trial sleeping a whopping 57.5 minutes later per night with treatment; it is not yet available for clinical use in the USA.
Melatonin and Kids with ADHD
Attention deficit hyperactivity (ADHD) is commonly associated with sleep problems, just as sleep problems can cause attentional issues. As many as 70% of children with ADHD may have sleep problems. Sleep problems include difficulty falling asleep, abnormalities in sleep architecture (e.g. the proportions of different stages of sleep), and daytime sleepiness. Trials of melatonin (in doses ranging from 3–6 mg) showed that it helped children with ADHD to fall asleep more quickly, although there was no evidence of improvement in attentional symptoms during the day. Side effects reported included problems with waking up at night and daytime sleepiness in some children. There is a nice review article here.
Delayed Sleep Phase Syndrome and Melatonin
Delayed sleep phase syndrome (DSPS) is a common disorder in teens, where their natural sleep period is shifted significantly later than the schedule which their commitments (usually school) mandates. Thus, teens with this disorder an unable to fall asleep by 1–2 AM in the morning or even later. I have seen kids who are routinely falling asleep between 4–5 AM. Melatonin has a clear role in this disorder, as small doses 3–4 hours earlier than sleep onset (along with light exposure limitation, sleep hygiene measures, and gradual changes in schedule [chronotherapy]) can be effective in managing this disorder. The reason for the delay is a marked delay in the DLMO, so melatonin dosing can move sleep periods earlier. For children with DSPS, giving a dose 4–6 hours prior to the current time of sleep onset, then moving it earlier every 4–5 days, is recommended, with low dose preparations. Of all the conditions mentioned here, this has the clearest benefit from melatonin. Here is a terrific review article.
Children With Neurodevelopmental Delay and Melatonin
Children with various causes of neurodevelopmental delay may have significant insomnia and melatonin may help. However, in some children melatonin use caused persistently high daytime blood levels of melatonin (and daytime sleepiness).
Blindness and Melatonin
Some children with blindness may have issues with sleep wake time as they do not have light regulating their circadian clock and may thus develop sleep disorders. Very small trials in adults have shown benefit (here’s one) but the data is very limited.
Eczema and Melatonin
Eczema is associated with dry, itchy skin and kids with it can have problems with insomnia and non-restorative sleep. Some research has suggested that children with eczema may have low melatonin levels, and a recent trial suggest that melatonin may be helpful.
It sounds great. Why should I worry about melatonin?
There are several areas for concern, specifically known and theoretical side effects, and problems with preparations.
- Side effects (known): In the short-term, melatonin seems to be quite safe. Unlike many other sleep inducing agents, “no serious safety concerns have been raised” (from Bruni review below). The most common side effects include morning drowsiness, bedwetting, headache, dizziness, nausea, and diarrhea. These effects are generally mild, and in my practice only the morning drowsiness seems to be significant. It can also interact with other medications (oral contraceptives, fluvoxamine, carbemazepine, omeprazole, and esomeprazole, to name a few).
- Side effects (theoretical): Melatonin given to children may lead to persistently elevated blood melatonin levels throughout the day. This can be associated with persistent sleepiness, but the other effects are unclear. It is important to know that melatonin has NOT been tested as closely as a pharmaceutical as the FDA regulates it as a food supplement. The studies following children who have been using melatonin long-term have relied mostly on parental reports as opposed to biochemical testing. A physician in Australia named David Kennaway has published two editorials this year pointing out the inadequacy of information on long-term use in children. (You can read this here). He states his point of view in a pithy fashion]”
…parents should always be informed that (1) melatonin is not registered for use in children, (2) no rigorous long-term safety studies have been conducted in children and by the way (3) melatonin is also a registered veterinary drug used to alter the reproduction of sheep and goats .”
- Problems with preparations– poor labeling:Melatonin preparations have been shown have to variable concentrations from preparation to preparation. Moreover, the amount that a child’s body absorbs may vary. Remember how I told you that melatonin was treated as a food supplement by the FDA?

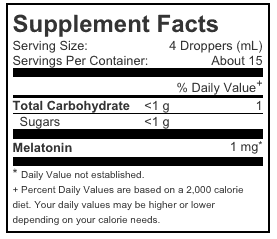
This means there is substantially less regulatory oversight in terms of safety and efficacy. I also find that the labelling of preparations is frequently misleading. Take the example of this liquid preparation, which many of my patients have tried. It is labeled as “1 mg” but each dropperful contains 0.25 mg.
You need to go to the web to get this information as it is not on the bottle. (It may be in the package insert, but I suspect few people read these).
A 2020 study of the PedPRM long acting melatonin formulation followed 80 children for 2 years, and did not show any evidence of effects on weight, height, body mass index, or Tanner staging (a measure of sexual development). This is the best long term study of melatonin safety and is quite reassuring.
My child is already on melatonin. Do I need to freak out?
I don’t think so, as there is little concrete evidence of significant harm. However, if you started melatonin on your own I beg you to discuss it with your child’s physician to see if it is really necessary. If your child has been using it long-term and sleeping well, you can consider slowly reducing the dose and seeing if it is still really necessary. Try to use it as needed as opposed to nightly. Also, I would take a hard look at sleep hygiene and ensure that you are ensuring good bedtime processes such as a high quality bedtime routine and avoidance of screen time for at least an hour prior to bedtime. I would try to reduce the dose, and potentially only use it as needed as opposed to nightly.
My doctor and I have talked about it. What should we consider regarding how and when to give melatonin?
Melatonin can be a tricky medication to dose. Effects change depending on when you give it compared to your child’s usual sleep schedule. Thus, a small dose a few hours before bedtime can have more of an effect than a large dose given at bedtime. In some situations (as with people whose sleep schedules may be flipped to a daytime sleep schedule) dosing may the opposite effect. This is a special case and should be addressed with your physician. A couple of rules of thumb.
What is the dose of melatonin for children?
Here is how we use melatonin in our clinic. (You should discuss melatonin with your pediatrician before dosing it.) In our clinic we follow the dosing recommendations in the Bruni article. We use a maximum dose of 3 mg for children less than 88 lbs 40kg. and 5 mg for children more than 88 lbs /40 kg. Often kids come to my clinic on higher doses– if 10 mg doesn’t work, sometimes lower doses or a different preparation work better! Also remember, not everyone responds to melatonin. Recognize that melatonin, unlike other medications, is a hormone, and that lower doses are sometimes more effective than higher ones, especially if the benefit of it reduces with time.
For assistance with sleep onset, usually dosing 30-60 minutes before the desired bedtime is best. I usually start at 1 mg and increase by 1 mg every 3-5 days to the maximum dose . Some children will actually do better with an earlier dose– for example, around dinnertime. So you may want to vary this a bit. If one mg works, you might want to see if you can get away with less.
For shifting sleep schedules later (as in delayed sleep phase), the dosing is different. You definitely want to work with a sleep doctor for this. That being said, we usually start with 0.25-0.5 mg four hours before bedtime and titrate up by 0.5 mg until you get a benefit.
Here’s the critical part. Melatonin is not a substitute for good sleep hygiene practices and should only be used in concert with a high quality bedtime, limitation on light exposure, and an appropriate sleep schedule.
When possible, purchasing a USP Verified preparation may indicate that the product is manufactured to the requirements of the U.S. Pharmacopeial Convention, which could mean that the quality controllers are tighter. The brands I have had the best luck with are Pure Zzzs, Natrol, and Zarbees. (Full disclosure– I did some consulting with Proctor and Gamble around the launch of Pure Zzzs but have no ongoing relationship with this product line).
What is the take home? Should my child take melatonin?
I have not met a parent who is eager to medicate their child. Such decisions are made with a lot of soul-searching, and frequently after unsuccessful attempts to address sleep problems via behavioral changes. Treatment options are limited. There are no FDA-approved insomnia medications for children except for chloral hydrate which is no longer available. Personally, I use melatonin for children commonly in my practice. It is very helpful for some children and families. I appreciate Dr. Kennaway’s concerns but I have seen first hand the consequences of poor sleep on children and families. I always investigate to make sure that I am not missing other causes of insomnia (such as restless leg syndrome). My end goal is always to help a child sleep with a minimum of medications. I know that this is the goal of parents as well. Some children, especially those with autism of developmental issues, will not be able to sleep without medication. So, melatonin may be a good option for your child if:
- Behavioral changes alone have been ineffective
- Other medical causes of insomnia have been ruled out
- Your physician thinks that melatonin is a safe option for your child and is willing to follow his or her insomnia over time
By the way, here’s a great article from the Chicago Tribune on alternatives to melatonin.
One other thing- if your child’s sleep difficulties came out of the blue, perhaps you are dealing with a sleep regression. Here’s what you can do.
So, this has been quite a long post. Do you have questions about melatonin use in children and teens? What has your experience been?
A special thanks to Bob Young R.Ph (aka the legendary “Bob from Pharmacy”) for his assistance with this.
- If you would like more information on this I recommend this Cochrane review on the topic, and this WebMD article.

- An age appropriate bedtime was defined as 8:30 PM + 15 minutes x (age in years – 6). These children had had problems for at least a year for at least four nights per week.

- The initial trials both used 5 mg around 6 PM. A later trial tried multiple doses. Interestingly, the dose did not matter, and the lowest dose (0.05 mg/ kg of the child’s weight) was equally effective. [So, for a 40 lb child– 40/2.2 = 18. 2 kg. 18.2 * 0.05mg/kg = 0.91 mg].

-------------------------------------
By: Craig Canapari
Title: Melatonin For Children? A Guide for Parents
Sourced From: drcraigcanapari.com/should-my-child-take-melatonin-a-guide-for-parents/?utm_source=rss&utm_medium=rss&utm_campaign=should-my-child-take-melatonin-a-guide-for-parents
Published Date: Sun, 03 Oct 2021 18:24:46 +0000
.png)